What does Betahistine do to you?

What Does Betahistine Do to You: How it Works, Its Benefits, and Side Effects
If you suffer from vertigo, the spinning sensation can leave you grabbing the nearest surface, waiting for the world to stop moving. For many patients dealing with vestibular disorders like Meniere’s disease, betahistine offers a treatment option that can provide stability and relief. This histamine analog has been helping people manage vertigo symptoms for decades, but understanding exactly what betahistine does to your body can help you make informed decisions with your healthcare provider.
Whether you’ve just been prescribed betahistine or you’re researching options to relieve your persistent symptoms, this guide will walk you through everything you need to know about how this medication affects your body, when to expect results, and what side effects you may experience.
Key Takeaways
- Betahistine improves blood flow to your inner ear and reduces vertigo symptoms by acting on histamine receptors
- Common effects include reduction in dizziness and tinnitus (ringing in your ear) intensity within 2-3 weeks
- Side effects are typically mild and including nausea (16% of users), headaches, and stomach upset
- The medication works by blocking H3 receptors and stimulating H1 receptors in your inner ear
- Most people tolerate betahistine well with withdrawal rates similar to placebo (16%)
- Effects on hearing loss are minimal – betahistine primarily targets balance and vertigo symptoms
How Betahistine Works
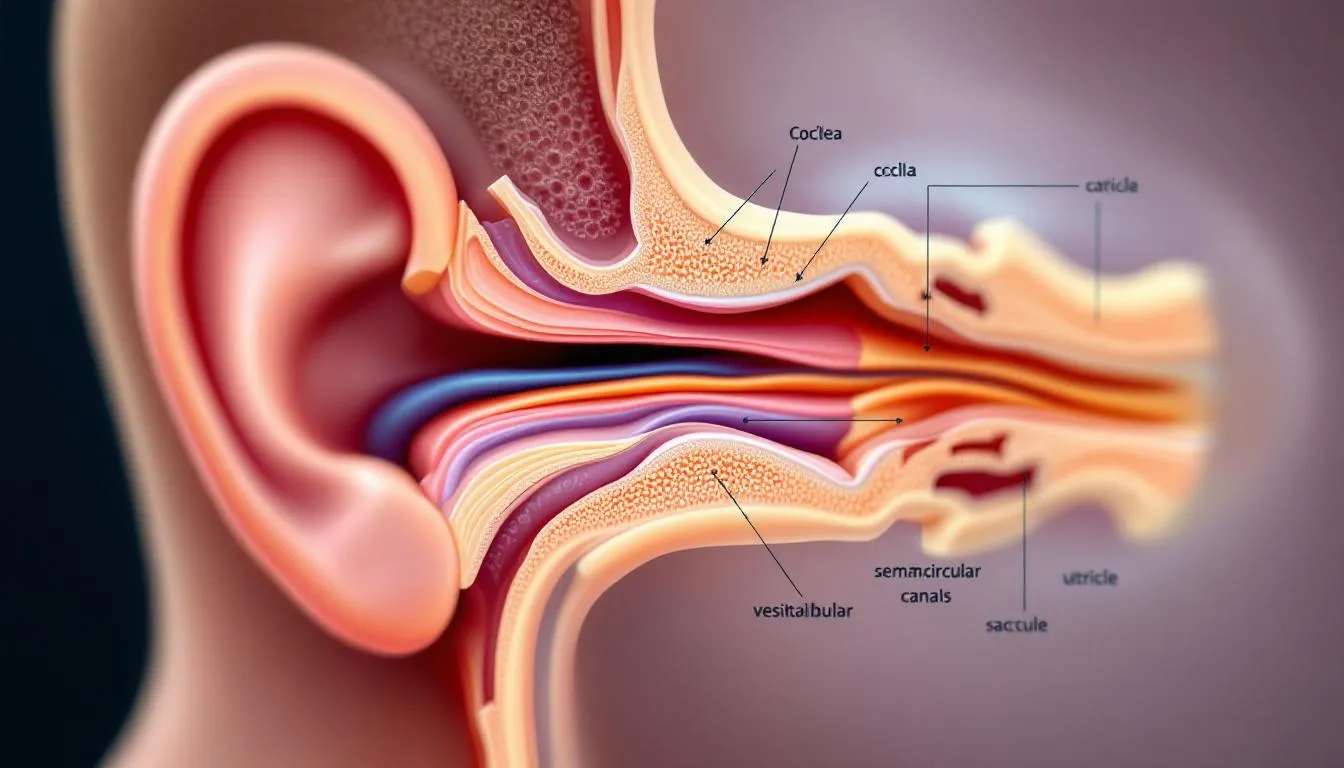
Betahistine dihydrochloride functions as both a weak histamine H1 receptor agonist and a strong H3 receptor antagonist, creating a dual action that specifically targets the root causes of vestibular vertigo.
When you take betahistine, it acts directly on the tiny blood vessels within your inner ear to improve blood flow. This increased circulation helps reduce the buildup of fluid that often causes the dizziness and balance problems associated with Meniere’s disease and other inner ear disorders.
The drug also crosses the blood-brain barrier to influence activity in your brainstem. By blocking H3 receptors, betahistine increases the release of several important neurotransmitters, including histamine, acetylcholine, serotonin, norepinephrine, and GABA. These chemical messengers work together to restore proper balance signaling between your inner ear and brain.
Some research suggests betahistine may even have mild cognitive effects through improved cerebral blood flow, though the significance of this is not fully understood.
What Effects You May Experience
The most noticeable change many patients report when taking betahistine is a reduction in the frequency and intensity of vertigo episodes. Within days to weeks of starting this drug, you might find that the spinning sensation becomes less severe and occurs less often.
Improved balance and stability during daily activities is another common benefit. People commonly describe feeling steadier on their feet and experiencing less of that unsettling sensation of false movement that characterizes these disorders. This improvement can significantly impact your quality of life, allowing you to return to activities you may have avoided due to balance concerns.
For those dealing with tinnitus, betahistine often provides relief from the constant ringing in ears that accompanies many vestibular conditions. While the drug doesn’t cure tinnitus entirely, many patients notice a reduction in the intensity and frequency of these sounds.
The medication also helps reduce the sensation of ear pressure and fullness that commonly occurs with Ménière’s disease and other inner ear disorders. This aural fullness can be particularly bothersome, and betahistine’s ability to improve fluid balance in the inner ear often provides welcome relief.Overall coordination and improved balance typically improve as the drug takes effect. People report feeling more confident moving through their environment and less concerned about sudden onset of vertigo.
Timeline of Effects

One of the most common questions patients ask is: “How quickly will I notice the benefits of betahistine?” This will vary among individuals, depending on the frequency and severity of your vertigo.
Initial improvements typically become noticeable within 1-2 weeks of starting betahistine. However, it’s important to understand that betahistine doesn’t provide immediate relief like some acute vertigo medications. Instead, the drug works gradually to address the underlying mechanisms causing your symptoms. Full benefits typically develop after 2-3 months of consistent use. This is because betahistine gradually increases blood flow to your inner ear and helps fix any damage or dysfunction.
Some patients notice dramatic improvements from common symptoms within the first 14 to 21 days, while others may need several months to experience the full positive effects of this drug. For chronic conditions like Meniere’s disease, long-term use may be necessary to maintain symptom control. This is why consistent daily dosing is so important to achieve the best results.
Common Side Effects of Betahistine
Understanding the possible adverse effects of betahistine will let you know what to expect when starting treatment. Fortunately, systematic reviews have shown that betahistine is typicaly well-tolerated, and side effects aree usually mild and easily manageable.
Gastrointestinal (GI) effects represent the most common side effects, occurring in approximately 16% of patients. These include nausea, upset stomach, and mild indigestion. Taking betahistine with food can reduce these stomach-related side effects.
Nervous system effects are less common but can include headaches and occasional drowsiness in some patients. Unlike many other medications used for vertigo, betahistine rarely causes significant sedation, which makes it preferable for long-term management of vestibular symptoms. Most side effects are temporary and go away as your body adjusts to the drug. Clinical trials have shown that the overall adverse event rate for betahistine (15-16%) is similar to placebo, indicating it is tolerable for most people.
When side effects do occur, they’re typically manageable through simple adjustments like taking the medication with food, adjusting the timing of doses, or working with your doctor to modify the dosage. You should avoid driving and doing other tasks or actions that call for you to be alert if you feel dizzy while taking this medication. The withdrawal rate from betahistine due to adverse effects remains low, with most patients able to continue treatment successfully.
If you experience a skin rash, hives, or signs of allergic reactions while taking betahistine, contact your doctor right away or seek immediate medical attention.
Dosage Effects and What Happens at Different Doses

The standard adult dose of betahistine is 16mg three times daily (48mg per day). This dosage has been used in clinical trials and has been shown to be effective and tolerable for most adults. Many doctors will start you on a lower dose of 8mg and gradually increase to a higher dose that works for you. This approach helps minimize potential side effects while allowing your body to adjust to the medication. The tablet form is most commonly prescribed, though oral solutions are available for patients who have difficulty swallowing pills.
Consistent daily dosing is important for maintaining steady levels in your system. Missed doses can lead to a return of vertigo symptoms, which is why it’s crucial to follow dosage instructions carefully and take the medication as directed by your doctor. The response to this drug varies significantly among individuals. While many patients achieve excellent symptom control, betahistine doesn’t work equally well for everyone. Some people may require alternative treatments or combination therapy for optimal management of their symptoms.
Higher doses don’t necessarily provide better control or your vertigo. Research has shown that taking higher than the recommended 48mg daily dose does not offer any additional benefits and may increase the risk of adverse effects. If you feel your current dose isn’t providing adequate relief, discuss alternatives with your doctor rather than increasing the dose on your own.
Taking betahistine with food is strongly recommended to reduce stomach upset and to ensure consistent absorption.
Long-term Effects of Betahistine Use
For patients with chronic inner ear disorders, understanding the long-term effects of betahistine is important. Unlike some medications, betahistine doesn’t appear to lose effectiveness over time. Many patients see relief from their vertigo with continued use, and there’s no evidence of tolerance development requiring dose increases.
Regular monitoring is recommended for patients on long-term therapy, though this is primarily to assess symptom control and treatment effectiveness rather than to watch for serious adverse effects. Your doctor may periodically review your response to treatment and adjust the regimen as needed.
Stopping betahistine typically leads to a gradual return of original symptoms rather than any withdrawal syndrome. You should never stop taking this medication or change your dose without first talking with your doctor.
Interactions and Precautions
When taking betahistine, there are several important interactions and precautions to consider. Alcohol can worsen dizziness and balance problems, so limiting alcohol consumption is generally recommended during treatment. The combination or alcohol and betahistine can also increase your risk of falls and injuries.
Drug interactions can affect betahistine’s efficacy or increase side effects. Antihistamines may reduce betahistine’s effectiveness by blocking the same receptors the drug targets. Monoamine oxidase inhibitors (MAOIs) can possibly increase betahistine’s effects or side effects. Always inform your doctors and pharmacist about every prescription medication and over-the-counter drug and supplement you’re taking.
You should not take betahistine if you have certain medical conditions. Those with severe bronchial asthma should avoid the medication, as it can potentially worsen breathing problems. People with pheochromocytoma, a rare tumor that affects blood pressure, should not take betahistine due to potential heart effects. Active peptic ulcers represent another contraindication, as betahistine’s histamine activity can increase stomach acid secretion and your risk of ulcers. If you have a history of stomach ulcers, discuss this with your doctor before starting treatment.
Pregnancy and breastfeeding safety hasn’t been adequately studied, so talk to your doctor if you are pregnant, planning pregnancy, or nursing. Your doctor can help weigh the potential benefits against unknown risks in these situations.
FAQ
How quickly does betahistine work? Most patients notice improvements within 1-2 weeks of starting treatment, though full therapeutic benefits typically develop over 2-3 months of consistent use. The drug works gradually rather than providing immediate relief.
Can I stop taking betahistine suddenly? While sudden discontinuation is generally safe and doesn’t cause withdrawal symptoms, it’s best to consult your doctor before stopping. Gradual discontinuation may be recommended to make sure symptoms do not return and any adjustments can be made.
Will betahistine make me drowsy? Drowsiness is uncommon with betahistine compared to other anti-vertigo medications. Most patients can continue normal activities without significant sedation, making it suitable for daytime use and long-term management.
Can I take betahistine with food? Yes, taking betahistine with food is actually recommended. Food significantly reduces the risk of upset stomach and other gastrointestinal side effects while ensuring consistent absorption of the medication.
Is betahistine addictive? No, there is no evidence of dependence or addiction potential with betahistine. The medication can be safely discontinued when appropriate without risk of withdrawal symptoms or dependency issues.
What if betahistine doesn’t work for me? If betahistine doesn’t provide adequate relief after 2-3 months of consistent use, discuss alternative treatments with your doctor. Options may include vestibular rehabilitation therapy, other medications, or combination approaches tailored to your specific underlying conditions and symptoms.
Understanding what betahistine does to you helps you to make informed decisions about your treatment. While individual responses vary, this drug has helped many patients regain stability and reduce the impact of vertigo on their daily lives. Work closely with your doctor to determine if betahistine is right for your specific situation and to monitor your response to treatment over time.